Relief From Pain
Research has linked hypnosis to pain relief, and recent studies suggest how this mind-body approach works to reduce pain. While undergoing MRI scans when patients were hypnotized prior to being touched with heat stimulus, as well as when the patients were not hypnotized, researchers found that hypnosis was successful in significantly reducing or eliminating pain in all 12 volunteers. Even more impressive was that the MRI scans showed that under hypnosis, activity was reduced in the areas of the brain responsible for pain perception. Research further suggests that hypnosis somehow blocks pain signals in the body from getting to the parts of the brain that perceive pain. (Regional Anesthesia and pain Medicine, November-December 2004)
After a full evaluation from your physician for the treatment of chronic pain conditions such as Migraine Headaches, Back Pain, Fibromyalgia, TMJ, Irritable Bowel Syndrome and many others, hypnosis is often recommended for additional treatment of the symptoms that interfere with daily activity. Jolene works closely with several Pain physicians to help improve your lifestyle and reduce your pain.
http://www.mayoclinic.com/health/hypnosis/MY01020/TAB=indepth
The release of endorphin (200 times stronger than morphine) as well as the muscle relaxation achieved during hypnosis can help to alleviate and even eliminate pain from chronic conditions. Jolene is uniquely qualified to help you manage your chronic pain condition not only as a chronic pain patient herself, but receiving her hypnosis training over a 12 year period at LDS Hospital Pain Clinic.
At the completion of hypnosis therapy (usually 6-8 sessions), you will receive audio recordings of each session to help reinforce the relaxation habit and release endorphin daily. You will further receive training during group classes to teach you the process of self-hypnosis so you can continue to manage your condition over time. You might also like to research further Hypnosis and Pain Management studies:
- Regional Anesthesia and pain Medicine, Vol 29, No. 6 (November-December), 2004: pp 549-556
- Journal of Clinical and Experimental Hypnosis, 53(2): 198-228, 2005
- Journal of Anesthesia and Analgesia: June 2002, Pain Control with hypnosis and Rapid Recovery
- Digestive Diseases and Sciences, Vol 47, No. 11 (November 2002)
- Prevention/ The Healing Power of Hypnosis
- Hypnosis for Chronic Pain Management and Medical uses of Hypnosis
- Pain Management Health Center (WebMD website)
Hypnosis Shows Long-Term Improvements In Refractory Chronic Pain
Boston—Although challenging to master, hypnosis can play an important role as part of a multidisciplinary approach to pain management, even in patients with refractory chronic pain, according to a team of Japanese researchers. By creating what the investigators called “analgesic nonpain experiences,” hypnosis can assist in even the most stubborn pain cases, they said.
“I met a patient [with complex regional pain syndrome (CRPS)] at the beginning of my career in pain treatment, when cognitive-behavioral therapy (CBT) and other treatments were not so effective for those patients,” said Miyuki Mizutani, PhD, a clinical psychologist at Aichi Medical University, in Aichi, Japan. “However, I thought hypnosis might be effective and started to learn the technique.
“I’ve now been performing hypnosis for 18 years, and have found it very effective in those patients, though it can be difficult to administer in chronic pain,” Dr. Mizutani continued. “It takes time, and complete remission is not very common. However, our experience is that repeated analgesic experiences can lead to long-term improvements in chronic pain.”

The process of successful personalized hypnosis practice begins with patient selection. Study participants were chosen if they suffered refractory pain after undergoing multidisciplinary pain treatment. These patients were then introduced to a clinical psychologist.
The participants underwent analysis with the Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale and Pain Disability Assessment Scale. Observed biological and psychosocial factors were grouped into 10 domains; voluntary patient experiences during in-session analgesic experiences also were recorded.
The principal hypnosis procedure comprised a number of phases. “Before hypnosis induction, we speak at length about the patients’ pain experiences,” Dr. Mizutani explained. “At that time, the pain experience comes into their consciousness; and during the conversation, some part of their pain experience is changed.”
As part of the hypnosis process, the practitioner facilitated nonpain body sensations and muscle relaxation in the patient. As the trance deepened, the practitioner offered somatic suggestions such as breathing, proprioception and/or ideomotor responses. Patients in the study underwent biweekly or monthly 60-minute sessions.
Reporting at the 2018 World Congress on Pain (abstract PFR560), the investigators revealed that 121 patients agreed to hypnosis, whereas 40 declined; those who agreed to hypnosis were significantly more likely to be anxious. Of note, hypnosis was readily accepted by patients with certain chronic pain conditions, including phantom limb pain, cancer-related pain, headache or orofacial pain, and visceral pain (Figure). Patients who accepted hypnosis also were significantly younger than their counterparts who declined.
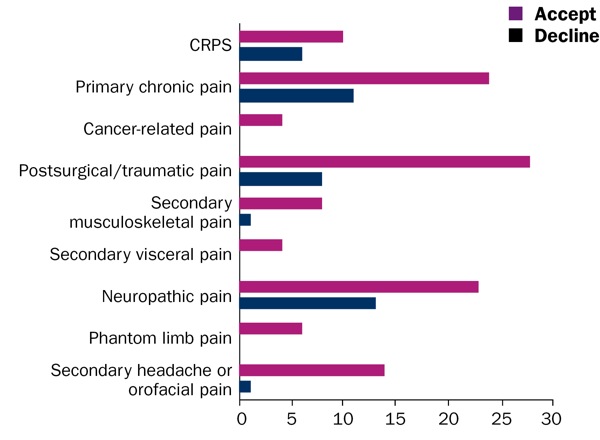
CRPS, complex regional pain syndrome; ICD-11, International Classification of Diseases, 11th Edition
To help quantify improvements in patient pain, the clinicians categorized their relief as “in-session analgesia” (relief occurring during a hypnosis session with a pain management practitioner) and “out-of-session analgesia” (relief that occurred extended into the patients’ daily lives).
The study found that 71% of patients who agreed to hypnosis (n=86) experienced in-session analgesia. Several factors found to be associated were successful in-session analgesia, including a greater number of years having suffered pain, lower scores on the Pain Disability Assessment Scale and lower levels of intrinsic motivation.
Among the patients who experienced in-session analgesia, 65% (n=56) saw their pain relief extend beyond the session, and were thereby classified as out-of-session analgesia. Among these, a lower number of biopsychosocial factor domains were significantly associated with successful out-of-session analgesia. These individuals also were significantly more likely to have mastered self-hypnosis, Dr. Mizutani added.
Treating the ‘Untreatable Part’ Of Chronic Pain
Despite these results, the researchers were quick to note that successful treatment of CRPS pain with hypnosis requires significantly more sessions than other forms of pain. Indeed, patients who experienced successful in-session analgesia required a mean of 3.75±3.85 sessions (range, one to 20). Those whose pain relief extended to out-of-session analgesia required a mean of 4.35±6.30 sessions after the first in-session analgesia (range, zero to 35).
Classifying exactly how hypnosis works for these patients is another challenge. As Dr. Mizutani explained, in-session analgesia is a distinct analgesic experience, and not simply an alteration of patients’ pain sensation or a distraction from their pain. “A nonpain experience becomes an analgesic nonpain experience when it shares the ‘neural network’ with the pain experience, competes with it, and wins it over in a focused and narrowed consciousness during hypnosis,” she told Pain Medicine News.
In the end, Dr. Mizutani believes hypnosis can be an important part of a multidisciplinary approach to treatment in people with chronic pain. “These patients have all undergone multidisciplinary pain treatment, including medication, physiotherapy and CBT,” she added. “And ultimately, they did not respond completely to those treatments. So we believe the untreatable part of the pain can be treated by hypnosis.”
A systematic review presented at the meeting (abstract PST451) demonstrated the efficacy of hypnosis in pediatric patients suffering from cancer pain. Investigators at St. Jude Children’s Research Hospital, in Memphis, Tenn., included a total of 17 articles in the review, comprising 12 randomized controlled trials and five non–randomized controlled trials with sample sizes ranging from 12 to 80 patients.
The analysis concluded that scientific evidence supports the preliminary efficacy of hypnosis in pain, distress and symptom management among youth undergoing cancer treatments. These benefits extended to procedure-related pain and anxiety as well as chemotherapy-related nausea and vomiting.
As Mark P. Jensen, PhD, a professor of rehabilitation medicine at the University of Washington, in Seattle, explained, most pain patients get at least some relief when employing hypnosis. “Hypnosis can be extremely beneficial for some patients, moderately beneficial for others and have limited beneficial effects in others,” Dr. Jensen said. “Almost everyone reports some benefit, however.”
Yet, as Dr. Jensen went on to discuss, there are several important considerations with such treatment, including the recognition that there is nothing “magical” about hypnosis. “When people are invited to focus their minds and are with someone they trust, they are more open to suggestions, and this includes suggestions for comfort, being able to ignore pain and experiencing improved sleep, among many others,” he said.
“It is also useful to remember that every patient responds differently to hypnosis treatment,” Dr. Jensen continued. “As a clinician, it is best to approach it with curiosity, wonder just how each patient will respond and try to maximize outcomes consistent with each patient’s goals. It’s useful to think of hypnosis as a skill set that patients learn to get more control over their own responses, including their pain responses.
“Finally, it is important for patients to obtain this treatment from someone who is a licensed health care provider,” he added. “There are many ‘hypnotherapists’ that have a hypnosis practice who are not otherwise licensed as health care providers.”
—Michael Vlessides
A surprise medical solution: hypnosis
The Wall Street Journal interviews UW Medicine gastroenterologist
According to The Wall Street Journal, medical centers are increasinglly using hypnosis to treat digestive conditions like acid reflux, irritable bowel syndrome and ulcerative colitis.
Most professionals who conduct hypnotherapy treatments are psychologists. Shoba Krishnamurthy, a gastroenterologist at the University of Washington, got training and decided to incorporate it into her practice about three years ago.
“It’s mostly for patients who have had a work-up but we haven’t found anything abnormal in tests, so there is not a specific abnormality to treat,” she says.
Studies have shown hypnotherapy is effective reducing symptoms associated with gastrointestinal disorders. Insurance companies usually cover the treatments. The body of evidence is strongest for IBS, but a 2013 study found hypnotherapy was effective at prolonging remission in colitis patients. And a 2016 pilot study found patients with functional heartburn reported fewer symptoms.
The treatment usually consists of about seven sessions over three months, with home practice in between. Studies have found the effects can last more than a year and work in more than half of patients.
Experts theorize that hypnotherapy works because many gastrointestinal disorders are affected by a faulty connection between the brain and the gut, or digestive tract. The gut and brain are in constant communication. When something disrupts that communication, the brain misinterprets normal signals, which can cause the body to become hypersensitive to stimuli detected by nerves in the gut, causing pain. Experts believe hypnosis shifts the brain’s attention away from those stimuli by providing healthy suggestions about what’s going on in the gut.
For further information about Pain Relief and the use of Hypnosis or to schedule an appointment, please call Jolene for a phone or in office appointment at 801-942-6175 or email joleneshields@yahoo.com
Click here to download your first Relief From Pain session.
Disclaimer
**Multiple hypnosis sessions may be needed to obtain your goals with hypnosis. Call to schedule an individual session, customized to your unique needs. Hypnosis is never a replacement for regular medical treatment. Hypnosis is often best used in conjunction with other wellness processes to achieve your desired results and outcomes. Please never listen to your download while driving or operating mechanical equipment.**
